How Much Does Chantix Cost With Blue Cross Blue Shield
Most patients with Blue Cross NC health insurance also have a medication plan to cover the medications they get at their pharmacy. Each medication plan comes with a list (or formulary) that shows you what medications are covered.
Are your patient's prescription medications covered?
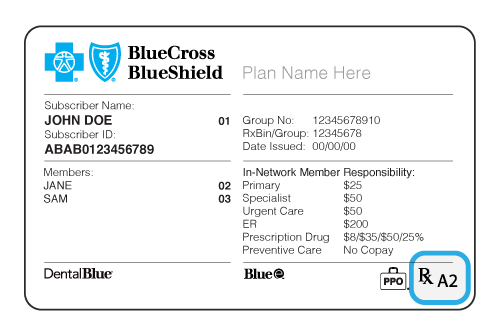
1) Look for the "Rx" on their member ID card. It means they have medication coverage.
2) Look for a capital letter or a capital letter/number combination after the 'Rx' on your patient's card. The letter will tell you which drug list, or formulary, your patient's plan uses. The number gives information about the pharmacies in your patient's network.
Enhanced Drug List
A, B,
Essential Drug List
C, D
Net Results Drug List
E
How to Find Your Patient's Approved Medication List or Formulary
1) Return to the Providers homepage
- Click Find Doctor / Drug / Facility on the top toolbar
2) On the Find a Doctor, Drug or Facility page
- Click the Find a Drug or Pharmacy tab
- Click Employer & Employee plans
- Answer Yes or No to the member ID card question
- Select the member's plan type from the menu
- Click See Drug Coverage
You'll go to Prime Therapeutics, our pharmacy benefit manager's website. Your patient's medication list, or formulary, search should look like this:

3) Type a medication name in the blue search box, select the formulation and strength you are prescribing and click Submit.
- The medication name, description and cost tier info will appear below the search tool under "Selected medicines." Additional details, such as generic availability and pricing, are found under "See all pricing options."
- If you need to request prior authorization or there are other special requirements, those should be listed here, too. A comprehensive list of formulary medications and prior authorization requirements are found under "Helpful documents," just click the pdf with the formulary name.
Medications that Need Prior Authorization
Some medications need additional information, in writing, from you before Blue Cross NC can decide if they will be covered. Our drug search tool shows the restricted medications our members use most, the requirements for approval, and the details you must send us to get them approved.
Enter a drug name in the search box to see if it needs approval before it's covered by a patient's plan.
Or click the first letter of your drug to view lists:
To find a drug, use the search above or select a letter from the list above.
Brand Drug Name: {{header}}
- Generic Drug Name:
- Benefit: ,
- Specialty:
- Prior Review Required On: ,
MN Prior Authorization: ,
- Quantity Limits Required On: ,
- Quantity Limits:
- Restricted Access/Step Therapy On: ,
- Restricted Access/Step Therapy:
- Nonformulary on: ,
- Nonformulary:
- Criteria: ,
- Fax Form: ,
- Note:
No results found for '{{header}}'
Prior Authorization
Providers must explain in writing why patients need a certain medication before Blue Cross NC can decide if it will be covered.
Quantity Limits
To encourage the proper use of prescription medications, Blue Cross NC may restrict the amount of medicine an insurance plan covers. This may mean taking fewer pills each day without changing the total strength of the medication.
Step Therapy
Blue Cross NC requires that patients first try a medication or device that is not restricted before a restricted medication will be approved. Patients may be covered for a restricted medication if providers tell Blue Cross NC in writing that:
The patient has already used the non-restricted medication and it wasn't effective in treating the condition; or
The provider thinks the non-restricted medication is likely to be harmful to the patient's health or not effective in treating their condition.
Non-formulary
A non-formulary medication is one that isn't on a patient's Blue Cross NC medication list. Not all medication lists or formularies have non-formulary medications. Providers must confirm that a patient has tried the medication(s) on their list first, and that they were ineffective or harmful. Also, any medication-specific clinical criteria must be met before approval (available in the Drug Search).
Specialty Drugs
May be used to treat a complex or rare condition, and are generally:
- Prescribed with special dosing or administration
- Prescribed by a specialist
- Significantly more expensive than alternative therapies
Specialty drugs are limited to a 30-day supply and patients must get them from an in-network specialty pharmacy, so their benefits will apply to the prescription. In-network pharmacy options vary based on the patient's plan benefits.
Important: If your patient has changed health plans, you may need to tell us that your patient has met the rules for their new plan.
For Patients with an Essential Medication List (Formulary): If your patient meets the Criteria for Approval of Restricted Products (pdf), and their list says that Prior Review (Prior Authorization) or Step Therapy is required for a medication, but the medication isn't in the Drug Search, please send a request to Blue Cross NC using this General Authorization Fax Form (pdf).
Requesting Medications Not on Your Patient's Approved Medication List (Formulary)
For fastest processing, please submit requests online using CoverMyMedsTM. If all details are submitted online and the request is approved, the member may be able to pick up their prescriptions at the pharmacy in less than 2 hours.
Other processing methods include:
- Fax: 800-795-9403
- Mail: Blue Cross NC, Attn: Corporate Pharmacy, PO Box 2291, Durham, NC 27707
Once we have all required information, we'll make a decision within 3 business days and notify you. Requests are processed within 72 hours, unless urgent.
Urgent requests are handled within 24 hours. An urgent request is when you believe a delay would seriously jeopardize the life or health of the patient, the patient's ability to regain maximum function, or would subject the patient to severe pain that cannot be adequately managed without the care or treatment requested.
If you want your patient to take a medication that isn't on the Essential or Net Results medication list, here's what to do:
- Consider if there's another medication they could take.
- Check to see if the new medication is on the medication list. If it's there, you're all set!
- If you still need the non-formulary medication, send us a request to approve the non-formulary medication.
- For approval, the patient must meet the Non-Formulary Exception Criteria (pdf). If the medication is listed in the Drug Search, these requirements may also apply.
- You must send all the details, with your signature, to Blue Cross NC.
- All requests can be submitted using CoverMyMeds or fax.
- If a medication is not listed in the Drug Search, request it using the General Authorization QL Fax Form (pdf)
- If the medication is listed in the Drug Search, use the fax form shown there.
- For questions, or to check the status of your review, call us at 1-800-672-7897.
For members on the Essential Medication List (formulary), if request for a non-formulary medication is approved, these cost levels or "tiers" will apply:
Essential 5 Tier = Tier 5
Essential 6 Tier = Tier 6
For members on the Net Results Medication List (formulary), if the request for a non-formulary medication is approved, these cost levels or "tiers" will apply:
Non-specialty medication = Tier 4
Specialty medication = Tier 5
Medications with Limited or No Plan Coverage
Some medications may not be covered by the patient's plan or may have a limited amount the patient can receive. The Table of Drugs with Limited or No Coverage shows a sample listing. Not all limited medications are listed.
For self-funded and ASO patients, you may need to call Blue Cross NC Customer Service for medication limits that may apply. If you are unsure if your patient's group is an underwritten or self-funded/ASO group, call the customer service number listed on the back of your patient's member ID card.
| Drug Type | Drug Limits |
|---|---|
| Infertility Drugs | For groups that, in 2013, had a $5000 lifetime maximum and were able to carry this over due to updates to the Affordable Care Act, this benefit will remain available. Otherwise, the benefit is as follows (call Customer Service to confirm): Underwritten and Individual/Family plans:
*Requires prior authorization before being covered |
| Sexual Dysfunction Drugs Related to Organic Disease (e.g., Cialis, Viagra, Caverject) | Underwritten and Individual / Family plans: Tadalafil (Cialis) 2.5mg or 5mg: 30 tablets per 30 days 4 tablets or units per 30 days |
| Sexual Dysfunction Drugs Unrelated to Organic Disease | All: Not covered |
| Prenatal Vitamins | Limited to members that are planning pregnancy, currently pregnant, or breastfeeding. If you believe you should qualify for an exception, please have your provider complete this form, and submit to Blue Cross NC for review. View the prenatal vitamin criteria for approval. In addition to the above benefit limitation, some prenatal vitamins are excluded from coverage entirely. These include, but are not limited to:
|
| Non-Food and Drug Administration (FDA) Approved Drugs | All: Not covered; please see the non-FDA approved medication and product list for specific medications that aren't covered |
| Initial fill of immediate-release opioid | All: Limited to maximum of 7 days for initial fill. If this is not the first fill, but Blue Cross NC does not have the patient's claims history, use this IR Opioid QL Criteria (pdf) and IR Opioid QL Fax Form (pdf). |
| Prescription medications with over-the-counter (OTC) alternatives | Please see member guide for coverage. Not covered as a standard benefit. Please see list for specific drugs that are not covered. |
| Medications used solely for weight loss | Please see member guide for coverage. Not covered as a standard benefit. Please see list for specific drugs that are not covered. |
| High Dollar Verification | Single claims over $10,000 require prior authorization (excluding antivirals, anti-infectives, anti-convulsants, insulin, specialty medications, and medications already subject to Prior Authorization or Step Therapy requirements). Criteria information can be found here, and fax submission information can be found by clicking here. |
Brand-Name Drugs vs. Generics
Don't let your patient over pay! They could be charged more if you prescribe a brand-name medication instead of a generic. If there's a medical reason the patient needs a brand-name medication, please:
- Check the Request for Waiver of Brand Drug Fees to see if your patient meets our requirements.
- Send a Safety MedWatch Form to the FDA tell them why your patient can't take the generic.
- Send us a Request for Waiver Faxback Form with your patient's details.
howardliferairipea.blogspot.com
Source: https://www.bluecrossnc.com/providers/medical-policies-and-coverage/prescription-drugs
0 Response to "How Much Does Chantix Cost With Blue Cross Blue Shield"
Post a Comment